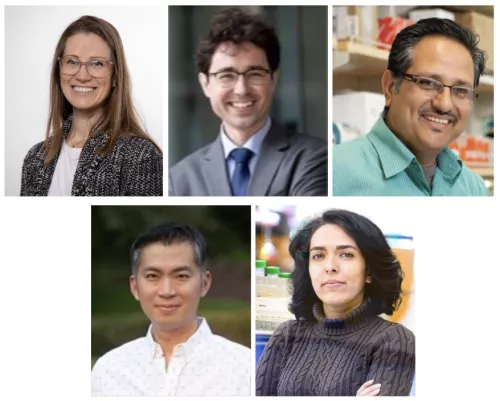
UCSF Broad Stem Cell Center Researchers received several grants from the California Institute for Regenerative Medicine (CIRM), the state’s stem cell agency, to fill in critical knowledge gaps in the biology of stem cells and regenerative medicine. Their projects advance approaches and stem cell-based technologies for treating brain vascular diseases, neurodegenerative disorders, retinitis pigmentosa, lung diseases, and gastrointestinal motility disorders. The Foundation Awards, given to Elizabeth Crouch, Tomasz Nowakowski, Deepak Lamba, Tien Peng, and Faranak Fattahi, were announced at a CIRM meeting at the end of March.
Harnessing vascular stem cells to grow and protect the human brain
Elizabeth Crouch, MD, PhD—Assistant Professor, Pediatrics
Dr. Crouch’s award will fund research to identify vascular stem cells in the developing brain and determine their impact on blood brain barrier formation. Brain vascular diseases can have profound impacts on long-term neurological function. Dr. Crouch’s project addresses critical gaps in our understanding of blood vessel cells in the brain, which impact one of the most vulnerable patient populations. Preterm babies born before thirty gestational weeks are prone to developing brain hemorrhages due to an unknown cause. The work will identify blood vessel stem cells to protect and harness them for regeneration after injury.
Identifying roadblocks to neural stem cell transplantation into human tissues
Tomasz Nowakowski, PhD—Associate Professor, Neurological Surgery
Dr. Nowakowski’s award will support his efforts to develop improved protocols for human neural stem cell differentiation, enhancing the fidelity, safety and robustness of future cell therapies. Cell therapy applications in the nervous system have the potential to address Central Nervous System (CNS) disorders, including epilepsy, stroke, and neurodegenerative disorders. However, neural stem cell transplantation into human brain tissue is inefficient and poorly understood. Dr. Nowakowski’s project directly addresses these limitations using a combination of genetic and cellular approaches.
Modeling Retinitis Pigmentosa using patient-derived human iPSC organoids
Deepak Lamba, PhD—Associate Professor, Ophthalmology
Dr. Lamba’s award will fund the development of a human retinal organoid model of autosomal dominant retinitis pigmentosa (adRP) to gain insights into pathogenesis and assess clinically relevant approaches to restore rhodopsin (RHO) protein function. Upon successful completion, the team will have established a disease-in-a-dish model and a novel therapeutic approach toward the management of the devastating outcomes in RHO-associated adRP. Retinitis Pigmentosa leads to devastating visual impairment in millions of individuals. Using the patient's stem cells, Dr. Lamba’s team aims to understand the disorder better and identify new therapies.
Ex vivo fate mapping of human lung stem cell plasticity in fibrotic disease
Tien Peng, MD—Associate Professor, Medicine
Dr. Peng’s award will support his efforts to generate new approaches to studying lung stem cells. This research could serve as a platform to discover drugs that will improve stem cell health in lung disease. The team will design new models to study behavior that is specific to human lung stem cells and screen for drugs that can target abnormal stem cells in fibrotic disease. Dr. Peng and his team aim to improve options for those with fibrotic lung diseases such as idiopathic pulmonary fibrosis.
hPSC-derived enteric ganglioids for cell therapy in gastrointestinal motility disorders
Faranak Fattahi, PhD—Assistant Professor, Cellular Molecular Pharmacology
Dr. Fattahi’s award funds will enable the generation, purification and characterization of enteric neurons from diverse hiPSCs and the assessment of their efficacy for cell therapy in gastrointestinal motility disorders. Her research addresses a significant unmet clinical need for a cell therapy approach for gastrointestinal motility disorders such as Hirschsprung disease, achalasia and gastroparesis. Gastrointestinal (GI) motility disorders are severe and common medical conditions resulting from dysfunction or degeneration of the enteric nervous system (ENS). The ENS is an extensive network of neurons inside the gut tissue responsible for the local regulation of motility and digestion. Dr. Fattahi’s work aims to develop stem cell-based therapies to replace the damaged or absent enteric neurons in motility disorders such as Hirschsprung disease, achalasia and gastroparesis.